Disorders & Treatments
After identifying and analyzing the location of the epileptogenic area, the multidisciplinary team mentioned before carefully assesses each patient in the joint conference. This team meeting enables the physicians to carefully review each patient and develop a treatment plan that may go beyond medical or surgical therapy and include social, psychological, and psychiatric services as well.
Medical Therapy
Medical management utilizes existing antiepileptic drugs in monotherapy and in rational polypharmacy. In addition, investigational pharmacologic agents are available for patients who do not respond satisfactorily to conventional antiepileptic drugs.
Surgical Therapy
Epilepsy surgery is recommended only after a thorough evaluation and only for patients who will significantly benefit from surgery. The efficacy of resective surgery for partial epilepsies is well documented. The surgery is safe and well tolerated, and the majority of patients experience substantial improvement, often gaining complete control of their seizures (seizure freedom). When resective surgery is not possible, partial corpus callosum section can relieve generalization of seizures and eliminate injury for some patients with generalized motor, tonic, or atonic seizures. Other special surgical procedures such as lesionectomy with intraoperative EEG monitoring, corpus callosotomy and multiple subpial transection (MST) are also available.
Surgical therapy is recommended after a comprehensive evaluation that includes continuous video EEG monitoring with scalp and sphenoidal electrodes, neuropsychological testing, and structural (MRI) and functional (PET, MRS, SPECT) brain imaging. In some candidates, localization of the epileptogenic region with this noninvasive evaluation is not sufficiently well defined so as to permit patients to proceed directly to surgery. In these cases, further evaluation with intracranial electrodes may be required.
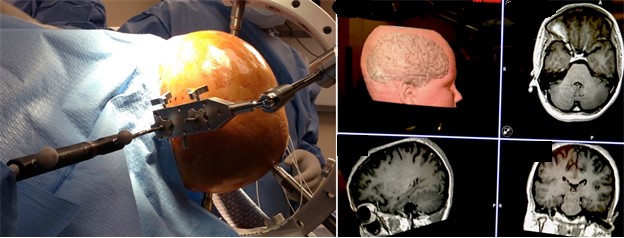
Intracranial electrodes are placed surgically in regions suspected to include the epileptogenic cortex. A variety of electrodes are utilized, depending on the information from pre-surgical evaluation and the regions of brain from which recordings are to be obtained. The intracranial electrodes include subdural or depth electrodes. Electrodes are placed through burr holes, craniectomies, or craniotomies, depending on the type of electrode used. Stereo EEG (sEEG) utilizing multiple depth electrodes inserted through tiny holes in skull can be placed to cover large part or much more detailed focuses evaluation in a particular region. This technique provides less morbidity and quicker recovery (see image). In addition to recording directly from the surface of the cerebral cortex, intracranial electrodes allow functional brain mapping to be performed. This ensures a safe resection by defining the margins of eloquent areas of the brain, such as speech, motor, and sensory cortex (see image below). Once the noninvasive and/or invasive studies have shown a well-defined focus of seizure origin, the patient becomes a candidate for surgery.

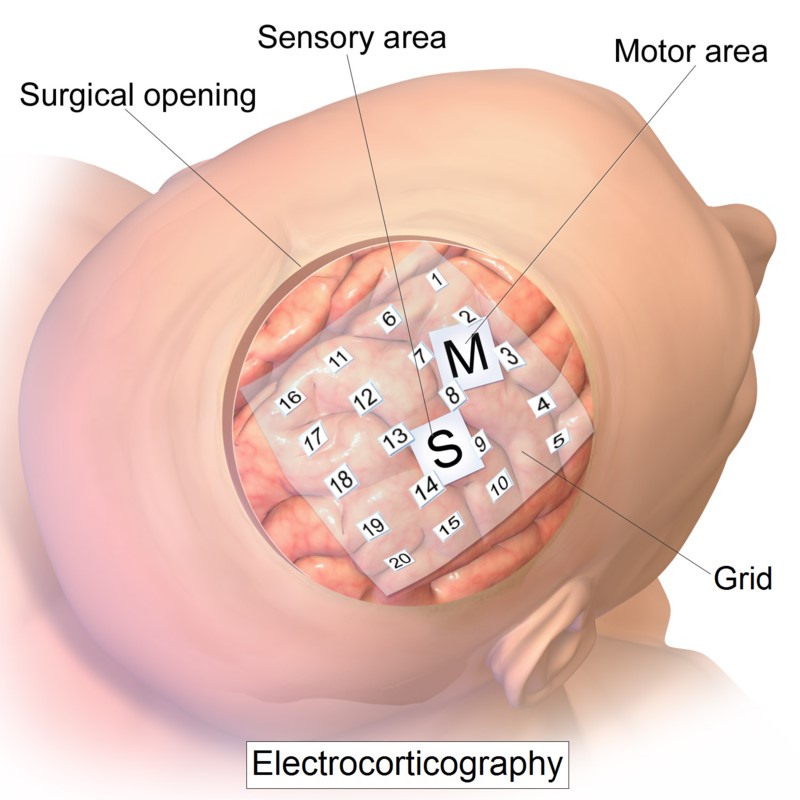
Example of Subdural Intracranial electrode placement.
At this time, all of the information obtained, including the anatomical information (MRI) and functional information (PET, MRS, SPECT, and video EEG recording), are gathered into a computer system and used for interactive image guided resection of the epileptogenic focus. Interactive image-guided surgery is done using a system developed by the Department of Neurosurgery at Wayne State University. This system consists of three infrared cameras that track the position of the surgical instruments. By these means, the surgeon is able to follow the margins of the epileptogenic focus and resect the structural and functional abnormalities. In some cases, when the epileptogenic focus is close to eloquent areas of the brain (speech, motor, sensory cortex, etc.), the surgery is performed under local anesthesia (the so called "awake craniotomy") with intraoperative functional mapping. The intraoperative electrical stimulation defines the functional areas such as speech, motor, and sensory cortex. The epileptogenic focus is then resected if it does not include any eloquent area of the brain. This technology insures a safe resection by defining the epileptogenic focus and avoiding any damage to eloquent cortex.
Vagus Nerve Stimulation (VNS)
For some patients who are refractory to medical therapy, we offer an implantable vagus nerve stimulating device that has been shown to reduce seizure frequency.
Responsive Neurostimulation® System
RNS or Neuropace is a system with electrodes implanted on or in the epileptogenic region of the brain. It can detect rudimentary seizures and provide real-time stimulation to reduce seizure frequency. Both RNS and VNS systems are programmable and requires a close follow-up with a specialist to monitor functioning of the device and programming changes to optimize the treatment.
Psychological and Psychiatric Services
Psychiatrists are available with special expertise in adult and pediatric epilepsy. Intervention may be on a one time basis for the patient alone or may involve family members as well. Ongoing treatment may be useful for some patients. Neuropsychological testing obtained prior to epilepsy surgery serves as a functional means of identifying the epileptogenic cortex and identifies neurocognitive deficits that would affect occupational and vocational rehabilitation.
Education/Support Services
Education is an integral part of the Comprehensive Epilepsy Program's mission. We offer ongoing education to help patients understand their condition and treatment options. Through a collaborative relationship with personnel from the Epilepsy Foundation of Michigan, we offer the additional services of medical social workers, nurse-educators, and psychologists.